You can read our most essential coverage of the coronavirus/covid-19 outbreak for free, and also sign up for our coronavirus newsletter. But please consider subscribing to support our nonprofit journalism.
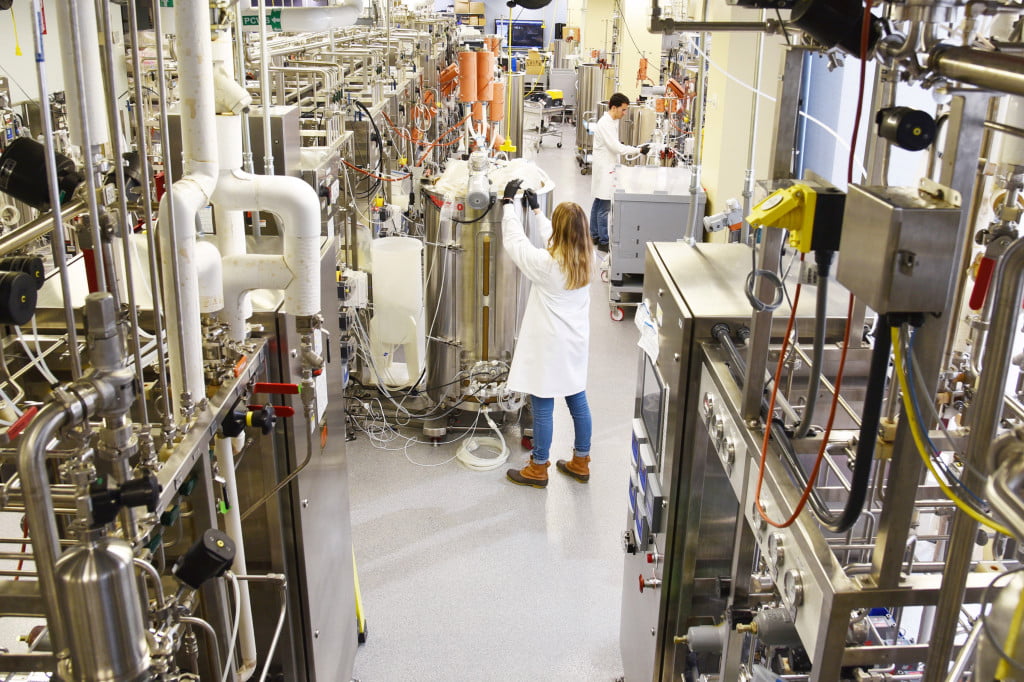
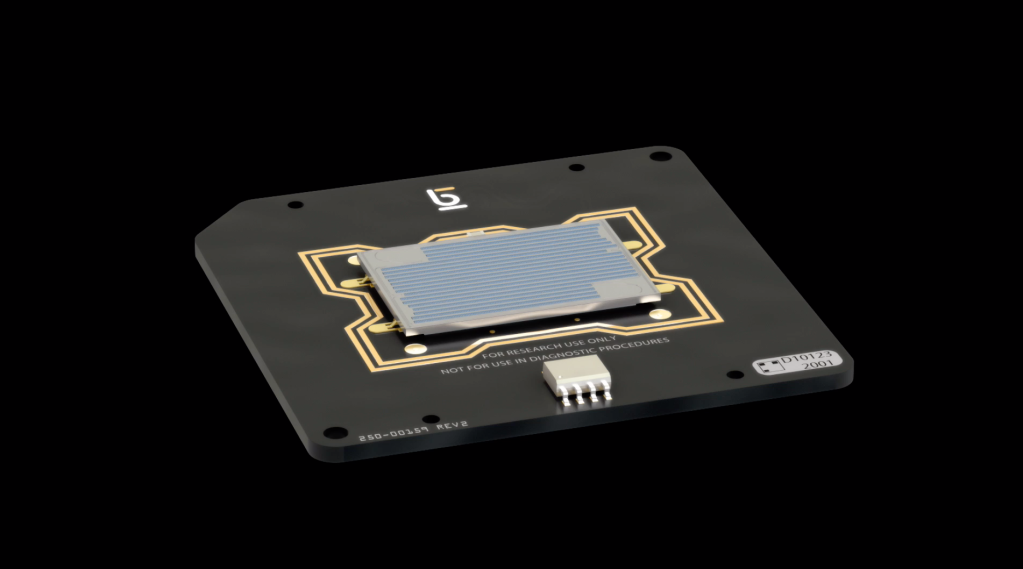
The company’s scientists quickly prepared the blood for analysis on a microfluidic chip where individual immune cells can be isolated and their antibodies studied. Within three days, AbCellara CEO Carl Hansen says, the company had inspected 5 million cells and found 500 different excreted antibodies that stuck to the “spike” protein of the virus, potentially blocking it. Any one of these antibodies could be a cure for others infected.
In the US, a slow and confused rollout of coronavirus testing helped the new virus get a foothold and cause what is now a raging outbreak. But drug and biotech companies have been searching for a cure since January, when the severity of the epidemic in China became evident. Among the most promising candidates are antibody drugs, a type that already accounts for most of the top-selling medicines in the US.
The goal of the companies looking into antibodies—which include AbCellera, Berkeley Lights, GenScript, Regeneron Pharmaceuticals, and VIR Biotechnology—is to turn one person’s solution to covid-19 into a drug that can benefit everyone. Antibodies can lock onto the virus and neutralize it. A dose given to the sickest patients could beat back the infection and lower the death rate. These drugs are not vaccines, but because antibodies last for weeks or months in a person’s blood, they could also act like a temporary vaccine—say, to protect health-care workers. If the right antibody can be found, manufactured, and bottled, it could be among the first treatments for covid-19.
That means blood from survivors is in high demand. The Rockefeller University in New York blasted out an email in mid-March saying, “Have you recovered from Coronavirus infection? If so, scientists need your help!” The center offered “compensation and parking” to anyone over 18. The National Institutes of Health (NIH) put out its own call days later.
Some US hospitals are collecting blood from survivors so the plasma in it can be directly transfused into patients with severe cases. The use of such “convalescent serum” was tried as early as January as an emergency treatment in China, with promising results. That’s not an ideal solution because serum, which has a large mixture of antibodies present in small amounts, is not as potent as a manufactured drug, and blood donations remain in short supply. Direct transfusions are “not scalable” as an answer to covid-19, says Rockefeller University immunologist Michel Nussenzweig. Still, the blood from patients who beat the virus is invaluable in the search for specific, powerful antibodies that can be identified and manufactured in a concentrated form so that “we can give them to other people … to a lot of people,” he says.
Despite the promise of antibody drugs, they may not yield a cure soon. Biotech companies say they will have antibody treatments ready for testing within two to four months, and possibly in larger quantities within half a year. That means none of the custom-designed drugs will arrive in time for the first wave of the pandemic, and they may not even be available in large amounts for the next phase, which in the Northern Hemisphere could happen next fall.
Says Nussenzweig, “The time line is similar to vaccines: it will take about year.”
Vaccines, pills, or antibodies
Antibody drugs are just one of the approaches being tried. Since the start of the covid-19 outbreak, drug researchers across the world have scrambled to find a treatment. Some have thrown open their libraries of chemicals; other have fired up deep-learning programs to predict what drugs could work. Immediately, doctors in China tried existing drugs, from herbal remedies to HIV medications. By mid-March, there were more than 250 clinical trials under way worldwide, and the World Health Organization (WHO) had launched Solidarity, a global mega-study of four readily available drugs, including one used to treat malaria. More than 60 potential vaccines are also in development.
In the face of widespread disease—and a death rate that, according to some recent studies, appears to be about 10 times that associated with the flu—all we have now are “non-pharmaceutical” measures. Countries are locking down—closing stores, airports, cafés, everything but essential jobs. The unprecedented campaigns of physical distancing and, in some countries, tracing infected people and their contacts are aimed at reducing the germ’s chance to move. But the economic price of these steps is already beyond calculation.
Any medicine able to shorten the duration of symptoms, or that proves effective in saving the lives of dire covid-19 cases, could ease the toughest trade-offs. If a drug shifted the balance of hope for those who end up on ventilators in intensive care units, we could get back to our jobs while protecting the lives of the weak, elderly, and unlucky. With a treatment that cut the death rate significantly, covid-19 might be a problem, but not an economic disaster.
Each major approach—conventional chemical drugs, vaccines, and antibodies—brings advantages and drawbacks. Pills are easy to make and easy to take, but none has yet been proved to work. Vaccines can give protection, but no one can predict when one will be available. (At a minimum it will take 12 to 18 months; 17 years since the world battled an earlier coronavirus, SARS, no licensed vaccine exists.) Antibodies, often given through an IV drip, have the disadvantage that they are complex to manufacture, but the advantage that they copy the body’s own solution. Among “de novo” drugs—those being designed specifically for this germ—expect antibodies to be among the first you hear about.
How antibody drugs work
Inside your blood system, countless immune cells circulate, each one endowed with a unique antibody. Think of the antibodies as sensors able to identify foreign substances, like germs or cancer cells. The immense diversity of antibodies, made possible by the reshuffling of DNA inside newly born immune cells, accounts for why people can stave off many threats never seen before. If one of the B cells made in the bone marrow recognizes a germ, it will start spewing out its antibody in huge quantities. The time it takes to mount a successful immune response is often about a week.
“You have the potential in your body to encode 100 billion different antibodies.”
AbCellera’s microfluidic technology captures individual B cells from a blood sample and segregates them into micro-chambers, where they can be probed 200,000 at a time. A single experiment can determine which of those cells are making antibodies capable of most strongly attaching to the spike protein of the coronavirus, which it uses to enter human cells. The cells making the best antibodies can be removed from the device to have their DNA, the instructions for making that antibody, read. “You have the potential in your body to encode 100 billion different antibodies,” Hansen says. “These cells are special because they recombine their DNA, and that’s what our technology is able to sort through, to find the one that can be a therapeutic.”
Learning from Ebola
How fast can an antibody for the coronavirus be found and start saving lives? The time line to beat, say experts, comes from Ebola, a bleeding disease caused by a virus that flared up in West Africa in December 2013. The disease was fatal about 65% of the time, so when it got into Liberia’s urban slums and even reached the US and Europe with airline travelers, the US began pouring millions into potential vaccines and drug treatments.
Regeneron was one of the companies tapped to develop an Ebola treatment. The company, based in Tarrytown, NY, has established a system for finding antibodies using mice genetically engineered with partly human immune systems. The mice are exposed to a pathogen “over and over again,” according to Christos Kyratsous, the company’s vice president for research on infectious disease, so they develop very potent, and entirely human, antibodies without needing blood from a survivor.
Regeneron rushed to create an Ebola antibody drug starting in late 2014, “but by the time we were done, the epidemic was waning, and we didn’t get a chance to use it,” says Kyratsous. It was an example of how drugs can come too late in an outbreak or fail to find a market at all. An antibody Regeneron developed for MERS, a coronavirus that can jumps from camels to humans and kills 30% of its victims, has never been tried on any patient, Kyratsous says. That disease, first spotted 10 years ago, is still so uncommon it’s been impossible to carry out a study.
“People think that if you enter a treatment center, you leave in a coffin.”
Interest in the Ebola antibody would have faded too, but then Ebola flared back up in 2018 in the Democratic Republic of Congo (DRC). “So then we had the drug ready to go,” says Kyratsous. In what public health experts say could be a model for how to battle covid-19, a trial was carried out involving 673 patients to compare four treatments.
It was less than a year later, Kyratsous says, in August of 2019, that he received a call saying the trial was being halted. It wasn’t a failure; rather, it was too much of a success. Regeneron’s antibody cocktail and one from the NIH (based on an antibody collected from a survivor of a 1995 outbreak) worked so well that it would be unethical not to give them to every patient. Only 34% of patients treated with the antibodies were dying. Among those who got the drug early, nine of 10 survived.
The drug promised a transformative effect. It made people with frightening Ebola symptoms less likely to hide from health workers. “People think that if you enter a treatment center, you’ll leave in a coffin,” Jean-Jacques Muyembe-Tamfum, director of the DRC’s National Institute of Biomedical Research, said in the British Medical Journal. “From now on, we will no longer say that Ebola is incurable … We have a great message: a treatment center is a place where you can recover and that you leave alive.”
Speeding up the chase
With covid-19, people want to hear that they can go back to work, and see friends and family, without putting elderly relatives at risk. A study of the Diamond Princess, a cruise ship that became an accidental coronavirus laboratory, estimated the overall death rate of people with covid-19 infection to be 1.3%. For people over 70, it’s five to 10 times as lethal. As Bruce Aylward, a prominent epidemiologist with the WHO, puts it, “This is one of the most serious diseases you will face in your lifetime.”
If the Ebola trial—carried out in under a year in a war-torn country—is the current record for testing an outbreak treatment, the world hopes to beat that mark now. Regeneron says it plans to pick two antibodies against the coronavirus, and the company’s billionaire founder and CEO, Leonard Schleifer, told President Donald Trump on March 2 that he could have supplies ready in the summer. “We anticipate, if all goes well, 200,000 doses per month can come out of our factory in New York, starting in August,” he said.
By that point an estimated 60,000 Americans could be dead from covid-19 even with strict social distancing measures in every state, according to projections from the University of Washington’s Institute for Health Metrics and Evaluation in April. There is intense pressure to accelerate the drugs’ development—to take corners at high speed, if not cut them altogether. But some experts say it’s not necessary to skip steps, something that could doom a drug later on. Instead, Ebola showed it’s partly a matter of spending 10 times the money to go twice as fast. “You don’t throw out the rules, but you shorten all the steps,” says Myron Levine, an infectious disease doctor at the University of Maryland, who has trained teams in Africa to run vaccine trials. “An accordion when extended is quite wide, but you push it together and it’s short. You don’t skip steps; you squeeze the accordion.”
As covid-19 has spread outward from China, desperate hopes have surrounded any treatment with even a chance of working. From his Twitter account, Trump touted malaria drugs based on the chemical chloroquine, even though the benefits of these are not proven, and the US took steps to make the pills widely available.
Covid-19 patients have also made pleas for drugs from their ICU beds, sometimes using social media to try to contact companies. One drug they are asking for is remdesivir, an experimental virus blocker made by Gilead Sciences that is also in clinical trials. After handing out hundreds of doses to severely ill patients on a “compassionate” basis, Gilead had to temporarily stop, citing “overwhelming demand.”
Yet remdesivir was a flop in the big Ebola study. And that shows you can’t tell what drugs actually work without doing a randomized controlled trial, as Anthony Fauci, the head of the National Institute of Allergy and Infectious Diseases (NIAID), has repeatedly said during White House briefings. That type of trial involves picking some people at random to either get a drug or not get it, and seeing if there turns out to be a difference.
That kind of data should be ready soonest for the available chemical pills, chloroquine and remdesivir, which are already being given to patients in organized studies involving thousands of patients. The large number of covid-19 cases means these studies could fill up quickly—and solid proof the drugs work, or don’t, could be in hand by summer.
One possible outcome, though, is that these pills will turn out to help only a little, falling well short of a cure. In that case we may need to wait for a vaccine or for purpose—built drugs, like antibodies or custom virus-blocking chemicals of the sort that ended up being able to stop AIDS.
Manufacturing project
If the pandemic continues to grow, anyone who discovers a new treatment will be hard pressed to make enough of it. That’s especially true for antibodies.
During the Ebola trial, each subject got doses as high as 150 milligrams per kilo of body weight—or about 10 grams in all. If a covid-19 antibody is created, millions of people could need it. That means antibodies would need to be manufactured literally by the ton, in a process that involves skimming the molecules from tanks of living cells and drying them into a powder. But the biomanufacturing industry has never been asked to create that much of anything. If there’s an antibody Manhattan Project, it would be to build factories big enough for the job.
The largest biomanufacturing facilities in the world cost $1 billion to set up and have as much as 150,000 liters of broths bubbling at once. Carnley Norman, a vice president of manufacturing at KBI Biopharma, which produces antibodies, estimates that one such megafactory might be able to make enough antibody for a million people each year. But what if we needed to treat 10 or 100 million—and what if high doses of several different antibodies were required? At the high end, Norman’s calculation then becomes staggering: we’d need more than 300 such plants, more than exist in the world today.
“If the pandemic goes completely unchecked, we are going to have a problem,” says Hansen. “If an antibody becomes the only way, we would have to do something very remarkable to treat hundreds of millions. There is a question about whether manufacturing scale-up can keep up with the outbreak.”
Quantities of a curative antibody might be severely restricted, leading to difficult decisions about who gets treated, and in what country. Doctors and drug companies—and governments—would have to decide. The sickest patients will need the drugs most, but antibodies work even better if given early on. Giving them prophylactically to health-care workers will be tempting too, especially if supplies are limited. According to Regeneron, just a tenth as much is needed to protect someone for a few weeks as to treat a very sick patient.
But all that’s only if we get a drug. And some believe the path to an antibody, like the path to a vaccine, is probably going to be difficult. “We have to worry about the efficacy and the safety, because this virus has unique features,” says Liusong Yin, who heads discovery of biological drugs at GenScript, a Chinese research company that has 50 people doing antibody screening. He says if the virus mutates, stopping it will demand more complex antibody cocktails that hit it in three or four places at once. And for severe cases, he worries, antibodies can sometimes make people sicker by contributing to a storm of immune activity.
Given such concerns, some voices are rising to say that science—and, by extension, clever biotechnology firms—should not make excessively optimistic claims. The trouble is that the virus isn’t well understood. Basic facts about it remain unstudied, including who is most vulnerable and why. Yet companies are pushing forward, which means biotechnology is being built on a foundation of scientific unknowns. In an editorial, Holden Thorp, editor of the journal Science, compared the undertaking to “fixing a plane that’s flying while its blueprints are still being drawn.” He knows that the efforts could fail: “I am worried,” he wrote, “that science may end up overpromising on what can be delivered in response to coronavirus disease 2019.”
But the alternative is that the plane crashes. And few racing to find a cure are ready to accept that fate.