Jason Bae, an urgent-care physician in Northern California, has been seeing covid-19 patients for almost a month. When he first started ordering coronavirus tests, around the week of March 9, his health-care system was quoting a 48- to 72-hour turnaround time from their third-party laboratory. But “even from the very beginning, a lot of tests would take five to six to seven days to come back,” he says.
Around that time, Bae developed a sore throat after being exposed to a patient who had tested positive. He self-isolated, stayed home from work, and got his covid-19 test through the Stanford Health system, which is separate from his employer’s health system. Stanford had built a testing facility in house, and the result came back in less than three days: negative.
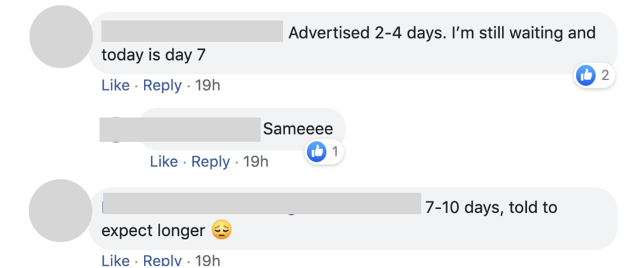
When he went back to work, Bae found that test results were coming back even more slowly than before, with many taking over a week. So on March 22, he posted in a private Facebook group of physicians to ask what his colleagues around the US were experiencing. The post drew over 1,500 replies. More than 40% indicated a turnaround time of seven days or longer.
Testing remains among the most pressing problems with America’s response to the pandemic. On March 31, the country announced that it has collectively tested a million people—weeks behind the schedule repeatedly promised by the Trump administration.
That is more than a mere statistic: testing people is the key to understanding how widely the novel coronavirus has spread and gauging its severity. Health-care workers need access to quick testing so that they can continue to safely take care of the rest of us. In the near future, we will also need testing to figure out how many among us may be immune and can get out of our houses and restart the economy.
You can read all our coverage of the coronavirus/Covid-19 outbreak for free, and also sign up for our coronavirus newsletter. But please consider subscribing to support our nonprofit journalism.
But as more and more Americans have been swabbed to test for covid-19, the lag between sample collection and the delivery of results is unpredictable. As the responses to Bae’s post show, some labs are handling the rise in demand worse than others.
In the responses, Bae found two distinct patterns. “The outpatient testing through the commercial labs is getting longer and longer,” he says, “whereas with the inpatient testing for hospitalized patients, the turnaround time has been coming down.”
In an effort to help understand the situation, Bae collected the responses in a spreadsheet. Analysis of his data reveals a patchwork system drowning in demand, but with some clear, fixable problems and signs of hope.
Who is doing testing?
There are currently four main types of labs performing coronavirus testing:
- the federally run Centers for Disease Control and Prevention, which initially handled all US testing (and was widely seen as a bottleneck early on in the outbreak)
- public health labs run by states
- in-house hospital labs that are part of a broader health system
- commercial labs, such as ARUP, BioReference Laboratories, LabCorp, Mayo Clinic Laboratories, Quest Diagnostics, and Sonic Healthcare, which now account for the bulk of testing volume throughout the country
While there currently isn’t any aggregate data on the number of in-house hospital tests done in the US to date, it’s likely a small percentage of the total. In Massachusetts, where there are many big academic hospitals, about 19% of all covid-19 tests completed have been done at in-house labs, while 65% have been performed at a commercial lab, according to figures published by the state’s health department. In most states, that figure is almost certainly much lower, as only the largest and best-appointed hospitals tend to have the resources to set up their own testing facilities.